Glaucoma Surgery
What is Glaucoma
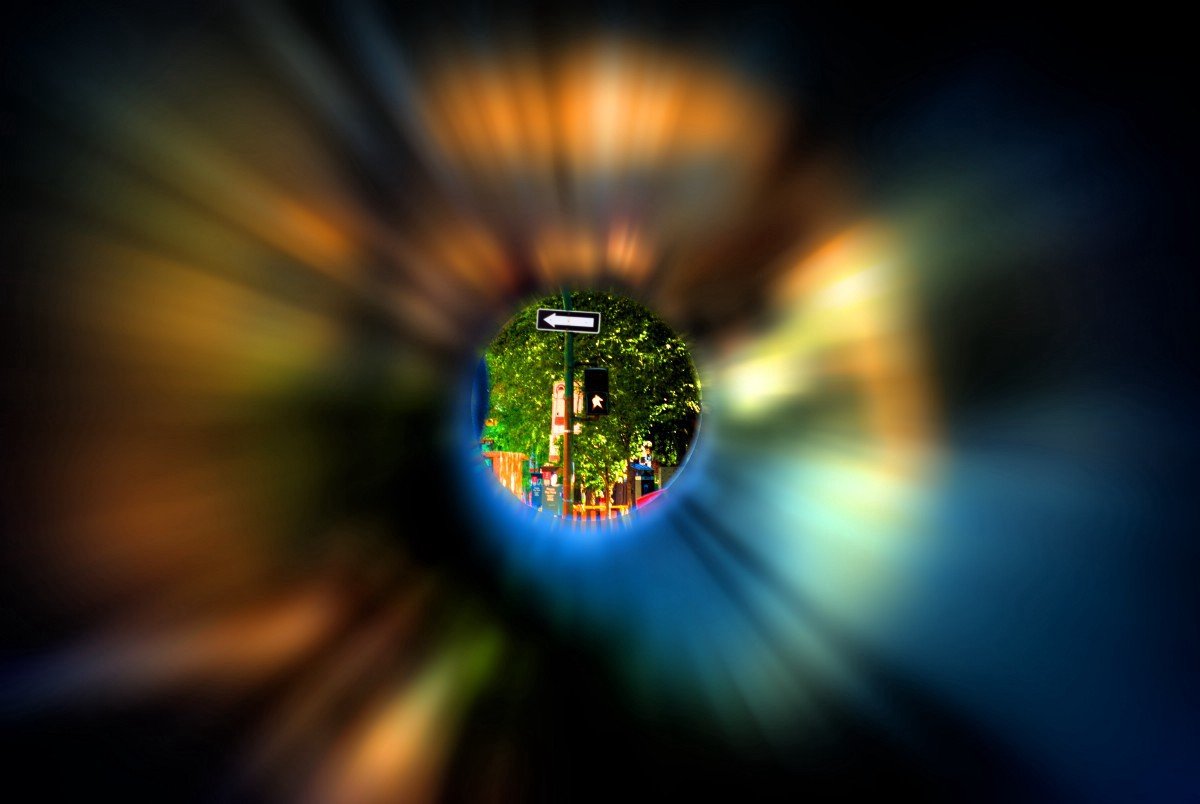
Glaucoma is a disease usually characterized by an increase in pressure within the eye. This may in time result in damage to the optic nerve, loss of peripheral or side vision and ultimately blindness. The higher the pressure within the eye, the greater the chance of damage to the optic nerve. Unfortunately, these symptoms are not always detectable in a patient, and glaucoma is a leading cause of blindness in the U.S., especially for older people. It is therefore important to have regular eye examinations.
Causes of Glaucoma
There are likely many factors working together which result in the disease called glaucoma. Increased pressure within the eye results from abnormal circulation of the clear fluid called aqueous humor. Aqueous humor is continually produced within the eye and constantly drains from the eye. If there is either an overproduction of aqueous humor or insufficient drainage of the fluid, pressure builds up within the eye and the optic nerve may be damaged. Recently, the circulation of blood to the optic nerve has been implicated as a possible important factor in the causality of glaucoma.
Is Glaucoma Preventable?
Glaucoma cannot be prevented. Although early detection and treatment by your eye care specialist are the keys to minimizing optic nerve damage and preventing blindness from glaucoma, the disease itself is not preventable.
Dr. Shultz and Dr. Chang can detect it by examination:
Measure intraocular pressure (tonometry)
Inspect the drainage angle of your eye (gonioscopy)
Evaluate any optic nerve damage (ophthalmoscopy) and optical coherent tomography (OCT Scanning)
Test the peripheral or side vision of each eye (perimetry or visual field testing)
Treatments for Glaucoma
In the office Dr. Shultz and Chang can perform Laser Surgery to reduce or eliminate the need for eye drops, which are the common treatment of Glaucoma. For patients that have difficulty using eyedrops, have allergies to eyedrops, do not have adequate control of their eye pressure with drops and or are planning to have cataract surgery, Dr. Shultz can perform Minimally Invasive Glaucoma Surgery (MIGS). Dr. Shultz is considered a pioneer in the field of MIGS. He has presented his results at major conferences and has multiple ongoing FDA clinical trials evaluating the most current technologies available.
In addition, there are now new implantable forms of medication that can be used and also inserted into the eye to reduce the need for daily eye drops.
What’s Minimally Invasive Glaucoma Surgery (MIGS)?
Three Types of MIGS:
MIGS procedures fall into three different categories according to how they achieve decreased intraocular pressure:
Improving your eye's natural drainage system, known as the trabecular meshwork (iStent inject, Hydrus, KDB Goniotomy, and OMNI Ab Interno Canaloplasty 360)
Redirecting excess ocular fluid outside of your eye (XEN Gel Stent)
Decreasing the production of ocular fluid within your eye (Micropulse Cyclophotocoagulation)
MIGS is a state-of-the-art minimally invasive glaucoma surgery that uses microscopic instruments to facilitate small incision surgery. It provides a safer option to reduce eye pressure than conventional surgery, with the added benefits of a higher success rate and faster recovery time.
The goal of MIGS procedures is to improve fluid drainage out of the eye in patients with mild to moderate glaucoma, reducing elevated eye pressure that damages the optic nerve. Clinical trials have shown that MIGS procedures achieve a significant decrease in eye pressure over periods up to 24 months, along with a decrease in prescription eye drop usage.
MIGS procedures are frequently performed in combination with cataract surgery for the appropriate patients. Dr. Shultz performs the following MIGS procedures: iStent inject, Hydrus, Kahook Dual Blade Goniotomy, OMNI Canaloplasty 360, XEN gel stent, and Micropulse Cyclophotocoagulation.
Durysta Implant
What is Durysta:
Durysta is a tiny dissolvable implant that is injected into the eye during an in-office procedure. Durysta automatically releases a medication called Bimatoprost. This helps reduce intraocular pressure (IOP) within the eye caused by glaucoma. It helps lower pressure for patients with open-angle glaucoma or high eye pressure. (ocular hypertension).
How does it work?
The aqueous humor is a transparent fluid containing low concentrations of protein. It provides nutrition to the eye and maintains the eye in a pressurized state. But in glaucoma patients, the aqueous humor may not drain properly. Because of this, the eye pressure (IOP) becomes elevated to harmful levels. Bimatoprost is believed to lower IOP by increasing the flow of aqueous humour through the trabecular mesh of the eye’s drainage network, or other uveoscleral routes.
How long does the implant last?
In clinical studies, Durysta lasted 4-6 months. Some ophthalmologists are reporting that their patients are continuing to experience lower pressure for 12-24 months. The implant should dissolve after about six months. Some researchers believe that it may create longer lasting positive effects in the trabecular network. There will be ongoing research on this topic. Currently, Durysta is only approved for a one-time treatment per eye. Repeat implants are not currently approved by the FDA.
What are the benefits of Durysta?
Most patients begin treatment of elevated intraocular pressure with topical drops. Unfortunately, a large number of these patients fail to achieve lowered pressure. They may not remember to insert their drops regularly, can’t afford the ongoing cost, or can’t tolerate some side effects.
With Durysta, patients don’t have to worry about whether they are administering the right dosing. The implant is an excellent alternative to daily drops, and many patients report that they are happy with their results.

